Suicide Prevention
For information on additional 24/7 crisis supports available, click here. |
|
If you or someone you know is experiencing thoughts of suicide, please reach out for help at 988 or 811. |
|
If you are worried about the immediate safety of yourself or someone you know, visit your local health care centre or call 911. |
- Overview
- Life Promotion
- Who Does Suicide Affect?
- How To Notice When Someone Might be Thinking About Suicide?
- How Can You Ask for Help When You Are Having Thoughts of Suicide?
- What Can You Do to Help Others?
- What Supports Are Available?
- What could it look like to reach out for support?
- Asking about Suicide in Healthcare Settings
- Self-Harm and Suicide
- How to Talk About Suicide
- Training Opportunities
- Funding Initiatives
- References
Overview
Suicide is difficult to talk about. Let’s talk about it.
The word suicide is used when someone ends their life on purpose. The reason people turn towards suicide is often complex, but there is always a way to support them. People who consider suicide as an option often don’t want to die, they are often looking for a way away from the pain they are experiencing. When someone talks about suicide, it is important to take it seriously.
There are many reasons why someone may be afraid to or avoid talking about suicide. These reasons could include:
- Negative stereotypes that are associated with suicide and mental health
- Fear of bringing bad things into existence by talking about them
- Not knowing what to say or being afraid of saying the wrong thing
- Not knowing if they are able to help the person in the way they want to be helped
Suicide does not only impact the individual who is having thoughts of suicide, but it also impacts those around them. It is important to look at the entire community as well as the individual when preventing suicide.
Some ways that we can take action to reduce suicide in communities include:
- Inspiring hope in our communities to prevent suicide (prevention)
- This could look like: learning how to recognize the warning signs of suicide and how to help; providing opportunities to increase connection to culture and others (i.e., learning language, traditional ceremonies and hide camps); and fostering personal skills such as coping, parenting, and relationship skills.
- Helping those who have thoughts of suicide (intervention)
- This could look like: having culturally safe mental health supports available (i.e., prioritizing Indigenous knowledge in services provided and addressing colonization and racism); providing suicide intervention training to community members; and creating holistic follow up plans for individuals.
- Supporting healing after a suicide has occurred (postvention)
- This could look like: planning cultural, traditional, and spiritual events that support healthy grieving processes through connection (i.e., fire feeding ceremonies and sharing circles); and providing additional supports for individuals impacted by suicide.
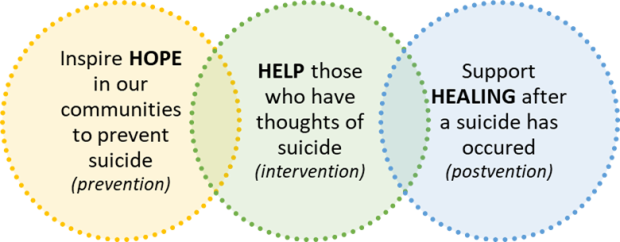
Adapted from: First Nations Health Authority
Life Promotion
Life promotion is a strengths-based approach that looks at the holistic well-being of Indigenous people and the communities. Life promotion focuses on creating a life that is meaningful and worth living for the individual to strengthen their connection to culture and life.
The First Nations Mental Wellness Continuum Framework defines mental wellness as the balance of the following aspects:
- “Spiritual wellness creates hope for their future and those of their families that is grounded in a sense of identity, unique Indigenous values, and having a belief in spirit.
- Mental wellness creates meaning and an understanding of how their lives and those of their families and communities are part of creation and a rich history.
- Physical wellness creates purpose in their daily lives whether it is through education, employment, care-giving activities, or cultural ways of being and doing.
- Emotional wellness creates belonging and connectedness within their families, to community, and to culture.”
Source: First Nations Mental Wellness Continuum
Suicide prevention aims to lower factors that increase suicide risk through different activities. Although, suicide prevention on its own fails to consider the unique life circumstances of Indigenous populations such as the ongoing impacts of colonization. An effective approach to preventing suicide needs to consider both suicide prevention and life promotion.
For resources related to life promotion, see below:
- Thunderbird Partnership Foundation
- Wise Practices for Life Promotion
- We Matter
- First Peoples Wellness Circle
Who Does Suicide Affect?
Suicide affects everyone, no matter their age, gender, income or culture. Some groups have different factors and system impacts that increase the risk of suicide (risk factors), but there are also strengths and different ways they are protected from suicide (protective factors). Just because these risk factors are present, doesn’t mean that suicide is bound to happen. These factors do not impact everyone in the same way.
Some factors that can increase and decrease the risk of suicide include:
|
|
Protective Factors |
Risk Factors |
Spiritual(Hope) |
|
|
Mental(Meaning) |
|
|
Physical(Purpose) |
|
|
Emotional(Belonging) |
|
|
Adapted from: Safety plans to prevent suicide for Indigenous young people and their caregivers, Centre for Suicide Prevention
For more information on these unique risk and protective factors, click here.
Some populations may be affected by suicide at a higher rate due to the ongoing and repeated impact of colonization, racism, transphobia, homophobia, sexism, and discrimination.
Historically within Indigenous populations, suicide was uncommon. After contact with European settlers and subsequent impacts from colonial practices such as: forced relocation, residential schools, loss of culture and language, the sixties scoop and discrimination, suicide has unfortunately become more common. The impacts of these events can be felt across generations, often termed has intergenerational trauma. As a result of the historical and current impacts from these experiences, Indigenous populations currently have higher rates of suicide than non-Indigenous populations. This is a normal response to these individual, intergenerational, community and systemic traumas that Indigenous peoples have experienced. Life promotion activities work to support Indigenous populations impacted by these events by using culture and connection as medicine. For more information on the differences between Indigenous and non-Indigenous groups, click here. For more information on indigenous peoples, trauma and suicide prevention, click here.
2SLGBTQIPA+ (Two-Spirit, Lesbian, Gay, Bisexual, Transgender, Queer and Questioning, Intersex, Pansexual, Asexual and Aromantic) individuals experience higher rates of suicide due to discrimination, victimization, rejection, and lack of access to affirming spaces. Some individuals who belong to two or more groups that experience these negative events can have a higher risk of suicide. One example of this is two-spirit individuals. Two-spirit individuals were held in high regard amongst Indigenous communities where they held sacred roles. This changed for many Indigenous peoples after contact with European settlers where European values were imposed on Indigenous communities. Resulting in discrimination, rejection, loss of culture and language, and increased suicide rates. For more information on suicide amongst 2SLGBTQIPA+ youth, click here or here and two-spirit individuals, click here.
For more information on the number of individuals impacted by suicide across Canada, please visit the Government of Canada’s website here.
How To Notice When Someone Might be Thinking About Suicide?
Reducing suicide depends on our ability to recognize people who might be thinking about suicide through warning signs. Warning signs are clues that can be used to recognize when someone might be thinking about suicide. These are based on what is commonly seen across the general population. Some individuals might experience one or more warning sign. It is also important to note that everyone experiences and presents with thoughts of suicide differently. When you notice these warning signs it is important to check in and ask if they need additional support.
Below is a list of common warning signs of suicide based on what it might look life, feel like, and sound like. This list does not identify all possible signs that an individual may observe, experience, or hear.
|
|
What it can look like:
|
|
What it can feel like:
|
|
|
What it can sound like:
|
How Can You Ask for Help When You Are Having Thoughts of Suicide?
If you are having thoughts of suicide, there are many ways to reach out for the help that you deserve. Some things that you can do to feel safer in the moment include:
- Recognize your thoughts of suicide.
- Reach out to someone in your life for support.
- Reach out to a professional for support (e.g., Elder, health care centre, crisis helpline, counsellor, 911).
- Remember what worked in the past or find new ways to manage strong feelings.
- Try to make your environment safer (e.g., remove weapons, substances, medications, sharp objects, chemicals).
- Be kind and caring to yourself, even when you don’t feel like it.
Asking for help is always right. Not sure if you need help? Learn more here.
For some examples on what you can do in the moment when the feelings become overwhelming, there are many exercises that you can try on your own or with someone you trust.
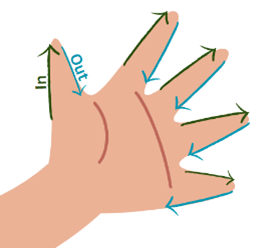
Breathing Exercise:
- Place your hand flat on a table or your lap
- Slowly trace the outline of your fingers starting at your thumb
- Breathe in as you move to the tip of your thumb
- Breathe out as you trace down your thumb
- Repeat with all your fingers
- Do this as many times as you need
Or visit the links below:
- Seven Sacred Teachings Grounding Exercises
- Daily Journal for Your Wellbeing
- What am I Feeling?
- Self-Care Medicine Wheel
- You are not Alone Colouring Book
What Can You Do to Help Others?
If you are worried about someone or they have let you know that they are experiencing thoughts of suicide, here are some things that you can do:
- Let them know that you care
- Ask them directly if they are thinking about suicide - Asking about suicide doesn’t make them more likely to think about it.
- Let them know that you’re here to listen without judgement
- Let them know help is available and create a list of supports based on their preferences (e.g., personal, cultural, and professional supports)
- Let them know that they are important and deserve support
- Make the environment safe (e.g., remove weapons, substances, medications, sharp objects, chemicals)
- Bring them to the nearest health care centre if there is immediate risk
- Keep yourself safe and identify supports for yourself.
Not sure what this could sound like? Here are some examples of things that you could say:
- “I care about you and I want to help”
- “I’ve noticed you haven’t been yourself lately.”
- “Are you thinking about suicide?”
- “Sometimes when people are going through similar things, they are thinking about ending their life. Are you thinking about that?”
- “It sounds like you’re carrying a lot right now”
- “I’m here to listen, can you tell me more about that?”
- “You’re not alone, there is help available”
- “You deserve help”
- “How can I support you right now?”
Remember, most of the time its not about what you say to the person, it is how you listened to them and made them feel.
For more information on how to be helpful when you are supporting someone who is thinking about suicide, visit the links below:
- Safety plans to prevent suicide for Indigenous young people and their caregivers, Centre for Suicide Prevention
- How to talk to someone you are worried about, 9-8-8 Suicide Crisis Helpline
- When a family member is thinking about suicide, Centre for Addiction and Mental Health
- Concerned about someone who may have thoughts of suicide, Canadian Association for Suicide Prevention
- Supporting a suicide attempt survivor, Canadian Association for Suicide Prevention
What Supports Are Available?
If you or a loved one are experiencing thoughts of suicide, help is available.
- Reach out to a friend, family member or elder for support
- Reach out to a professional for support
- Call your local Community Counselling Program
- Call the Trans Lifeline at 1-877-330-6366 (Monday to Friday 11:00 AM to 7:00 PM)
- Call a 24/7 Crisis Helpline
- 988 Suicide Crisis Helpline – Call or text 9-8-8
- Kids Help Phone – Call 1-800-668-6868 or text CONNECT to 686868
- Hope for Wellness Indigenous Helpline – Call 1-855-242-3310
- 811 NWT Helpline – Call 811 and press 1
- Indian Residential Schools Support Line – Call 1-866-925-4419
- Call 911 or visit your local health centre
For more information on supports available in your region, review your Regional Mental Wellness and Community Support Poster.
What could it look like to reach out for support?
Reaching out for help can feel overwhelming or scary – especially when you are not sure what to expect when you do reach out for help. Here are a few tips on what to expect when you reach out to the following supports:
- What to expect when talking to a friend or family member
- Sharing experiences with a trusted and safe person can often lead to feeling relieved and less alone in your experience.
- They can be there to listen to what you have been feeling and help connect you to other professional or cultural supports.
- If they are able to, they might also be able to support you alongside other professional or cultural supports.
- What to expect when calling a 24/7 crisis line
- Crisis Lines are confidential and anonymous supports that can provide a listening ear, coping skills for when you’re feeling overwhelmed and support to develop a safety plan.
- Crisis lines can help you if you are supporting someone with thoughts of suicide.
- Many crisis lines provide information on what you can expect when you call on their websites, including: 811, 988 and Kids Help Phone.
- In very rare cases, if a crisis line is worried about your imminent risk to safety that cannot be supported over the phone, they may inform an emergency service.
- Tip: It can be helpful to practice calling a helpline with a friend or support person when you are not feeling as overwhelmed. This can make it easier to call when you are having overwhelming feelings.
- What to expect when visiting a health centre
- They will ask a few more questions to better understand your experiences.
- They will help develop a safety plan.
- They might refer to other professional supports, such as a community counsellor.
- They might admit to a hospital if they worried about someone’s immediate safety.
Asking about Suicide in Healthcare Settings
Since anyone can have thoughts of suicide, care providers may also ask questions regarding suicide when providing services. This is something that is asked of everyone to improve our ability to identify and better support people who are having thoughts of suicide.
These questions that your care provider may ask you might sound like:
- “Over the past few weeks have you felt down, depressed, or hopeless?”
- “Over the past few weeks have you had thoughts of ending your life?”
- “Have you ever tried to end your life?”
You can also start the conversation around suicide with your care provider if you are having thoughts of suicide or are worried about someone who may have thoughts of suicide. Care providers can provide you information on what supports are available and help you in getting connected with these supports.
Self-Harm and Suicide
Self-harm is the intentional act of causing physical damage to oneself without wanting to die. Sometimes it might be difficult to tell the difference between self-harm and suicide. The way to tell the difference is by looking at the reason for doing the behaviour. Self-harm is a way to handle distressing feelings whereas with suicide it is used as a way to end their life. An easy way to tell the difference is by asking the person.
If you are unsure if it is suicide or self-harm, do not hesitate to talk to them about it and reach out for additional support. For information on what support is available click here.
If wounds from self-harm look serious or you are unsure, call 811, visit your local health centre or call 911.
For more information about the differences between suicide and self-harm and how to help, please visit:
- Self-harm and Suicide, Centre for Suicide Prevention
- Self-injury: What is it and how to cope, Kids Help Phone
How to Talk About Suicide
Being afraid of saying the wrong thing shouldn’t stop you from having the conversation about suicide. Although there are ways that we can change the way that we talk about suicide to make the conversation more supportive for the individual with thoughts of suicide. Asking about suicide doesn’t make them more likely to consider suicide. When we talk about suicide in a helpful and respectful way, we can begin to create a community free of stigma where we can talk more openly and safely about suicide. We can do this by using language that is person-first such as “experiencing thoughts of suicide” and neutral such as “suicide attempt”.
For more information on how to talk about suicide:
- Government of Canada - Language matters: Safe language and messages for suicide prevention
- Centre for Addiction and Mental Health – Words matter: Learning how to talk about suicide in a hopeful, respectful way has the power to save lives
Training Opportunities
If you are looking to build your knowledge around suicide and mental wellbeing the NTHSSA
offers the following workshops:
LivingWorks safeTALK
LivingWorks safeTALK is a four-hour training that equips people to be more alert to someone thinking of suicide and better able to connect them with further help. Using a simple yet effective model, safeTALK empowers everyone to make a difference.
Applied Suicide Intervention Skills Training
Applied Suicide Intervention Skills Training (ASIST) is a two-day interactive workshop in suicide first aid. ASIST teaches participants to recognize when someone may have thoughts of suicide and work with them to create a plan that will support their immediate safety.
Mental Health First Aid – Northern Peoples
The Mental Health First Aid – Northern Peoples (MHFA-NP) training course was developed to equip you with the tools needed to provide initial support to someone who may be developing a mental health problem or is experiencing a mental health crisis.
Contact us at SuicideNetwork@gov.nt.ca to request a workshop or if you need more information on figuring out what training would be the best fit for you.
Funding Initiatives
The GNWT provides funding opportunities to help build hope and healing within organizations and communities. For more information on what this funding is and how to access it, see below:
Community Suicide Prevention Fund
This program provides funding for community-based suicide prevention activities in the Northwest Territories.
Mental Wellness and Addictions Recovery Fund
This program provides funding for Regional and Community Indigenous Governments, Community Governing Authorities (Band Councils, Métis Locals, Charter Community, or municipal council) and Non-government Indigenous organizations to deliver culturally relevant, community-based options for individuals living with mental health and addictions in the Northwest Territories.
References
For more information on suicide:
- National Suicide Prevention Action Plan (2024 to 2027)
- Canadian Mental Health Association
- Centre for Addiction and Mental Health
- Canadian Association for Suicide Prevention
- Centre for Suicide Prevention
- Government of Canada
- Moving Forward, Healing Together Inuvialuit Settlement Region Suicide Prevention Strategy
- First Nations Mental Wellness Continuum Framework
- Inuit Tapiriit Kanatami Suicide Prevention Strategy
- My Voice My Choice – Self-Harm and Suicide Prevention
In addition to the organizations listed above, we would like to acknowledge the following partners who supported the development of this information:
- NTHSSA Mental Health and Community Wellness Division
- GNWT Cultural Safety and Anti-Racism Division
If you have any feedback, compliments or complaints on the information presented on this page, let us know by clicking here.